Abstract
Introduction and Objectives
Sickle cell disease (SCD) is a neglected tropical disease disproportionally affecting malaria endemic regions of sub-Saharan Africa. Estimated to affect up to 3% of the population in some areas, 50-90% of children affected with SCD die before age five due to lack of diagnosis and preventative care. Early screening and intervention improves survival, but is not the standard of care throughout much of the continent. Kenya, like several other sub-Saharan African countries, has piloted newborn screening (NBS) for SCD, but NBS programs based on the infrastructure and approaches in Western countries have proved challenging to replicate in resource constrained environments (RCEs). As many as 50% of patients who have screened positive for SCD in programs throughout Africa are lost to follow-up.
The recent development of affordable, point of care (POC) screening tests have provided an alternative approach to testing for SCD in RCEs. This study aimed to determine the validity and feasibility of utilizing a POC SCD screening test, HemoTypeSC™ (HTSC) in a RCE, to determine the prevalence of SCD in western Kenya, and to determine the rate of attendance at follow-up clinic after a positive POC screening test for SCD.
Methodology
Asymptomatic patients from birth through five years of age were approached for study enrollment in the pediatric vaccine clinic of Homabay County Referral Hospital (HCRH). 700 study participants were screened at HCRH over a 6 month period using HTSC. Isoelectric focusing (IEF) was run on a sample collected contemporaneously with the sample collected for testing with HTSC . At least one parent of each study participant was consented and counselled regarding SCD. Participants with a positive screen for either SCD or Sickle Cell Trait (SCT) were asked to return for confirmatory testing with Hb Electrophoresis (HBE). The HTSC screening results were compared to IEF and HBE results to determine the specificity and sensitivity, respectively. Samples yielding discordant results between HTSC or IEF and HBE were referred for molecular genotyping. Study participants with confirmed SCD were scheduled to attend a follow-up clinic. Participants unreachable by phone after at least ten attempts were declared lost to follow up.
Results
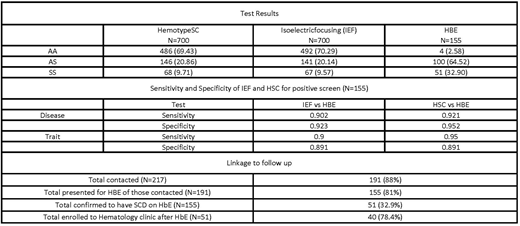
The median age of participants was 14 months (IQR: 5,30), 387(55.3%) were male. 18 patients had discordant results between screening tests and HBE and are pending molecular testing. 214 (30.6%) subjects screened positive for SCT or SCD on HTSC . 155 of these patients returned for HBE testing. The sensitivity of HTSC from the 155 receiving HBE testing was 92.1% for SCD and 95.0% for SCT. By comparison, the sensitivity of the concurrent IEF testing was 90.2% for SCD and 90.0% for SCT. The specificity of HTSC was 95.0% for SCD and 89.1% for SCT (as compared to IEF specificity of 92.0% and 89.1% for SCD and SCT, respectively). 9.6% of the subjects were found to have SCD, 20% had SCT. Of those with a positive screen for SCT or SCD, 191 (88%) were successfully contacted. 40 (78.4%) of those subjects confirmed to have SCD attended a follow-up clinical appointment. These data are summarized in Table 1. The majority of participants contacted who did not present for HBE testing or attend follow-up clinic cited socioeconomic factors as the main impediment.
Discussion and Conclusions
HTSC was found to be a feasible, valid POC screening test for SCD. The test was easy to perform and interpret, and facilitated prompt delivery of results. Education and counseling about SCD at the time of a positive screen led to a high rate of attendance at follow-up clinic. Further investigation is required to determine the long-term effect of POC testing on survival and quality of life outcomes. The prevalence of SCD in this cohort was among the highest rates reported in the literature. Though consanguinity was not documented as part of this study, it likely contributed to the high Hb SS frequency. These results support the notion that there is substantial regional variability in the frequency of Hb SS compared to national estimates extrapolated from Hb S frequency and highlight the criticality of more systematic, broad-based screening and treatment programs in targeted sub-Saharan African locations.
Wanjiku:Silverlake Research Cooperation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal